A Functional Movement Assessment (FMA) is valuable even if you're uninjured, as it identifies movement inefficiencies, imbalances, and potential injury risks.
By focusing on how your body moves, an FMA helps address underlying issues before they escalate into costly injuries or chronic pain, which could save you from expensive medical bills.
The assessment provides a personalized plan to improve mobility, strength, and stability, allowing you to self-manage your health and fitness.
This proactive approach empowers you to enhance physical performance and prevent long-term problems, promoting overall well-being without the need for frequent medical intervention.

A functional movement assessment identifies imbalances and limitations, helping to prevent injuries, improve mobility, and optimize performance through a corrective exercise programme.
Identify Movement Limitations
Detect Muscle Imbalances
Improve Posture
Reduce Chronic
Pain Risks
Track Progress
A client Functional Movement Assessment starts with a consultation. This consultation is a thorough discussion of the client’s health history, goals, and concerns, followed by an explanation of each assessment to ensure understanding and comfort.
This consultation is followed by:
1: Static Postural Assessment
Static postural assessments analyze the body's alignment while standing still, identifying imbalances, muscle tightness, and joint dysfunction.
This evaluation helps detect potential issues affecting movement efficiency, guiding corrective exercises and improving posture.

2: Movement Assessment
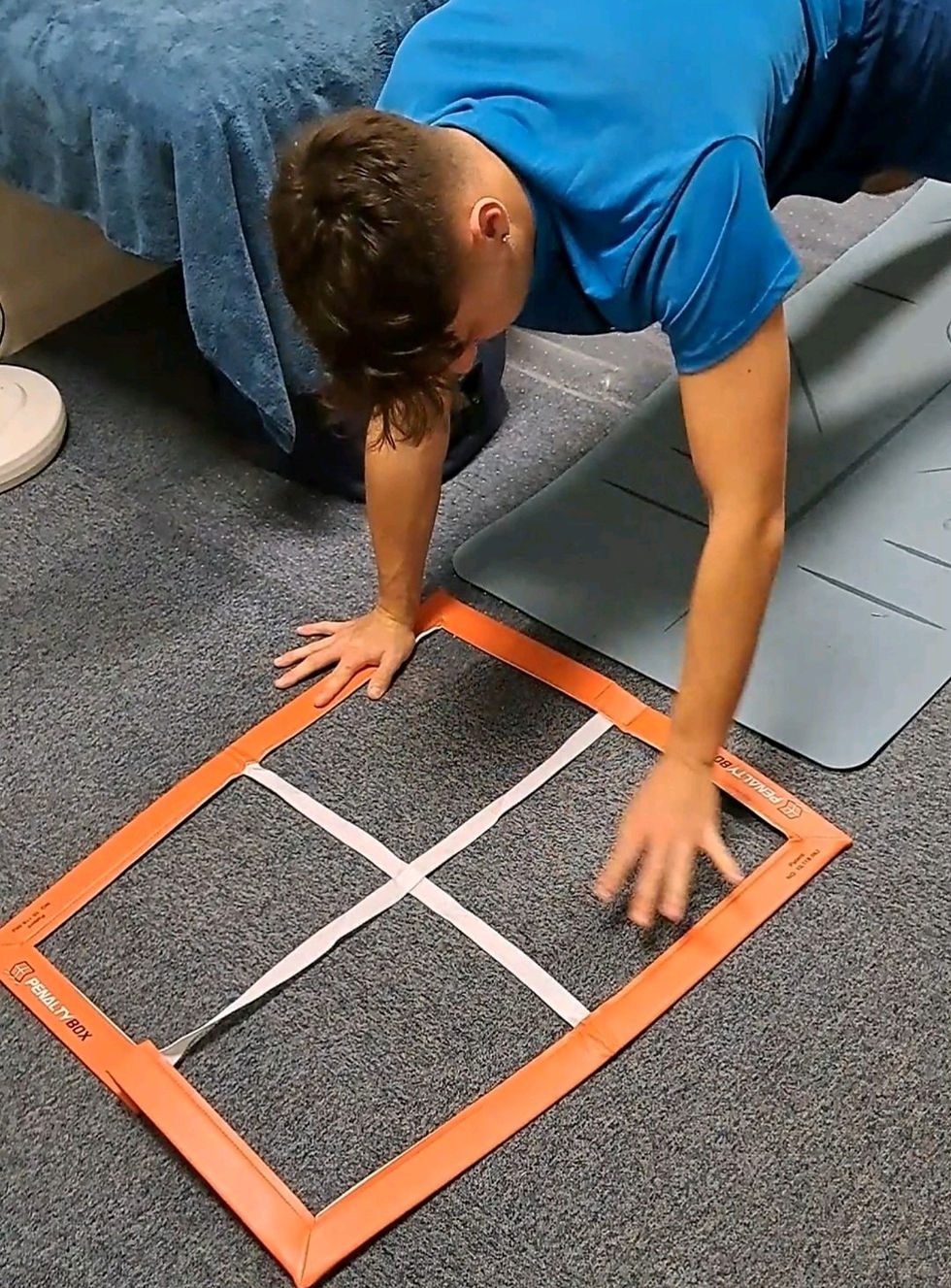
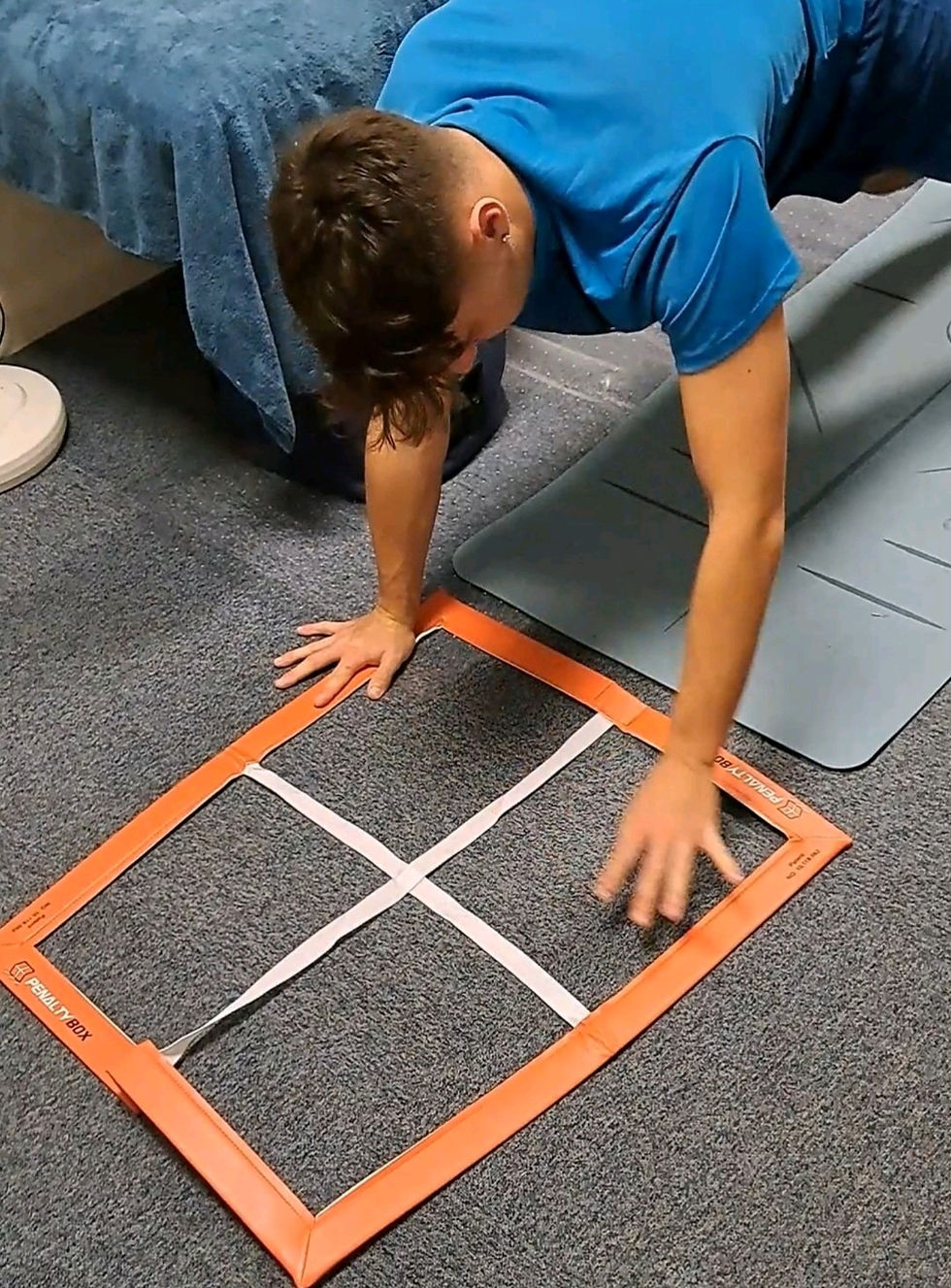
Functional movement assessments evaluate mobility, stability, and strength through exercises like the overhead squat and single-leg squat.
These tests reveal movement patterns, imbalances, and potential risk for injuries.

3: Mobility Assessment
The corrective exercise mobility assessment evaluates joint range of motion, flexibility, and movement quality.
It identifies restrictions or imbalances that limit mobility, guiding targeted exercises to improve flexibility, alignment, and overall functional movement.

4: Loaded
Assessment
Loaded movement assessments evaluate an individual's ability to perform fundamental movements, such as pushing, pulling, and overhead squats, under resistance.
These assessments help identify weaknesses, imbalances, and improper techniques, ensuring safer and more efficient movement patterns.
They are crucial for optimizing strength, stability, injury prevention, and overall athletic performance.

Kinetic Chain
Checkpoints
In functional movement assessments, the kinetic chain checkpoints are used to evaluate an individual's posture and movement quality to identify dysfunctions or imbalances.
These checkpoints focus on specific joints and segments of the body that are critical for optimal movement.
The main kinetic chain checkpoints include:
.png)
Head and Cervical Spine
Shoulders and Thoracic Spine
Lumbo-Pelvic-Hip Complex (LPHC)
Knee
Foot and Ankle
Key Focus:
Head and neck alignment relative to the shoulders.
Key Focus:
Shoulder positioning, thoracic spine mobility, and scapular movement.
Key Focus:
Pelvic tilt, hip rotation, and lumbar spine position.
Key Focus:
Knee alignment in relation to the foot and hip (especially valgus or varus positioning).
Key Focus:
Arch collapse (overpronation), external rotation, or flat feet.
Dysfunction:
Forward head posture or excessive cervical extension can lead to neck strain and affect overall posture and movement efficiency.
Dysfunction:
Rounded shoulders, scapular winging, or limited thoracic spine mobility can contribute to shoulder impingements, neck pain, and postural issues.
Dysfunction:
Excessive anterior or posterior pelvic tilt, lumbar lordosis (arching of the lower back), or hip instability can lead to lower back pain, hip issues, or inefficient movement patterns.
Dysfunction:
Knee valgus (knees caving inward) or knee varus (knees bowing outward), often related to foot or hip imbalances, can lead to increased stress on the knee joint.
Dysfunction:
Limited dorsiflexion, excessive pronation, or supination may lead to compensation throughout the kinetic chain, affecting balance and stability.
These checkpoints provide a framework for identifying movement dysfunctions and compensations that can impact performance, cause pain, or lead to injury. By analyzing these areas, corrective exercises can be designed to improve overall functional movement and reduce injury risk.


-
How long does a functional movement assessment take?A typical assessment takes 60 minutes, depending on the complexity of the movements being tested and the individual's needs.
-
What are the key movement patterns tested?Common movement patterns include: Squatting Lunging Pushing and pulling Rotating or twisting Gait (walking or running) Balance and core stability
-
What can a functional movement assessment reveal?It can reveal: Muscle imbalances or weaknesses. Joint restrictions or poor mobility. Poor coordination or motor control. Potential injury risks.
-
How often should I have a functional movement assessment?Frequency depends on your goals: Athletes or active individuals may benefit from quarterly assessments. During rehabilitation, assessments may occur more frequently. For general fitness, annual check-ins can track progress.
-
Do I need to prepare for a functional movement assessment?Preparation involves: Wearing comfortable sports wear, preferably shorts and for ladies a sports bra. Being ready to perform basic movements like squats or lunges. Informing the assessor about any injuries or pain beforehand.
-
Can a functional movement assessment improve athletic performance?Yes, it helps athletes by: Identifying and correcting inefficient movement patterns. Reducing the risk of sports-related injuries. Enhancing strength, speed, and agility through targeted training.
-
What is a functional movement assessment?A functional movement assessment is a series of tests used to evaluate how well your body performs basic movement patterns. It helps identify imbalances, weaknesses, or mobility issues that could lead to pain or injury.
-
Why is a functional movement assessment important?Functional movement assessments are crucial for: Identifying movement dysfunctions that may lead to injury. Creating personalized exercise or rehabilitation plans. Improving overall performance in sports or daily activities. Enhancing posture, strength, and mobility.
-
Who can benefit from a functional movement assessment?Anyone can benefit, including: Athletes aiming to enhance performance. Individuals recovering from injury or surgery. People with chronic pain or mobility issues. Those starting a new fitness program.
-
How is a functional movement assessment performed?I will guide you through specific movements or exercises while observing your posture, range of motion, and control. I may also use tools like video analysis or markers to measure your performance.
-
Are there any side effects or risks?Soft tissue massage is generally safe, but mild side effects like temporary soreness or fatigue may occur. Avoid massage if you have open wounds, fractures, or certain medical conditions (e.g., blood clots) without consulting your doctor.
-
Can soft tissue massage help with injuries?Yes, it can aid recovery by: Reducing inflammation. Breaking down scar tissue. Restoring flexibility and range of motion. Enhancing blood flow to injured areas.
-
What is soft tissue massage, and how is it different from other massage types?Soft tissue massage focuses on the muscles, tendons, ligaments, and fascia to relieve pain, improve mobility, and aid recovery. It includes various types like deep tissue massage (for chronic tension), sports massage (targeting athletic performance), and maintenance massage (for ongoing care).
-
Who can benefit from soft tissue massage?Athletes (for performance and recovery). Office workers (to relieve postural strain). Individuals recovering from injury or surgery. Anyone experiencing muscle tension, pain, or stiffness.
-
What is deep tissue massage, and who is it for?Deep tissue massage uses firm pressure to release tension in deeper layers of muscle and fascia. It’s ideal for: Chronic pain or tightness. Postural issues. Recovery from injuries like strains or overuse conditions.
-
What is maintenance massage, and how often should I get one?Maintenance massage is regular treatment to keep muscles healthy, reduce stiffness, and prevent injuries. The frequency required depends on your activity level and needs, but athletes or highly active individuals often benefit from sessions every 2–4 weeks.
-
What is sports massage, and how does it benefit athletes?Sports massage is designed for athletes to: Enhance performance by reducing muscle tension. Prevent injuries through improved flexibility. Aid recovery by promoting circulation and reducing soreness.
-
How long does a session last, and what should I expect?A session typically lasts 1hr. Expect: An initial consultation to discuss concerns or goals. Techniques like kneading, stretching, and trigger point release. Adjustments based on your comfort and feedback during the session.
-
Is soft tissue massage painful?While deep tissue or sports massage may involve discomfort when addressing tight areas, it should not be unbearable. A skilled therapist will adjust pressure to your tolerance and ensure the treatment is effective yet comfortable.
-
What’s the difference between pre-sports and post-sports massage?Pre-sports massage: Uses fast, stimulating techniques to warm up muscles, improve circulation, and prepare the body for activity. Post-sports massage: Focuses on calming muscles, reducing soreness, and accelerating recovery after intense physical activity
-
What should I expect during a rehabilitation session?A session may include: Initial assessment to track progress. Guided exercises targeting the injured area. Manual therapy to reduce tension or improve mobility. Education on activity modifications and self-care.
-
Can I do injury rehab at home?Some rehab exercises can be done at home, but professional guidance is crucial to ensure exercises are performed correctly and safely. Regular check-ins with a therapist can optimise recovery.
-
What are the common phases of rehabilitation?Acute Phase: Managing pain and inflammation. Subacute Phase: Restoring mobility and strength. Rehabilitation Phase: Functional training and advanced exercises. Return-to-Activity Phase: Gradual reintroduction to normal activities or sports.
-
Can injury rehabilitation help with chronic pain?Yes, rehabilitation can be effective for managing chronic pain by: Improving joint mobility and muscle strength. Reducing stress on affected areas. Teaching proper movement patterns and pain management strategies.
-
Why is injury rehabilitation important?Rehabilitation helps: Speed up recovery. Restore normal movement and strength. Prevent future injuries. Reduce pain and inflammation.
-
What is injury rehabilitation?Injury rehabilitation is a process aimed at restoring strength, mobility, and functionality after an injury. It often includes physical therapy, exercises, and other treatments to promote healing and prevent further damage.
-
How long does injury rehabilitation take?The timeline varies based on the injury's severity and type. Minor injuries may require a few weeks, while severe injuries, such as fractures or ligament tears, may take months to fully recover.
-
How can I prevent re-injury during rehabilitation?Follow your therapist's recommendations. Avoid pushing through pain. Focus on proper form and technique. Gradually increase intensity and load. Warm-up and cool down effectively.
-
What treatments are used in injury rehabilitation?Common treatments include: Physical therapy exercises. Stretching and strengthening routines. Manual therapy (e.g., massage, joint mobilisations). Modalities like heat, ice, or ultrasound. Education on posture and ergonomics.
-
When should I start injury rehabilitation?Rehabilitation often starts immediately after an injury, focusing on pain control and gentle movement. Delaying treatment can lead to stiffness, weakness, or chronic pain.
-
Can I do post-op rehab at home?While some exercises can be done at home, professional guidance ensures proper technique and prevents re-injury. Regular sessions with a therapist are often recommended during the initial stages.
-
When should I start post-op rehab?The timing depends on the type of surgery. For some procedures, rehab starts within a day or two, focusing on gentle movement. In other cases, it may begin weeks later, once healing has progressed.
-
What are the risks of skipping post-operation rehab?Without rehab, you risk: Prolonged pain and swelling. Loss of strength, mobility, and function. Development of scar tissue or stiffness. Increased likelihood of re-injury or complications.
-
What is post-operation rehabilitation?Post-operation rehabilitation is a structured recovery program designed to help patients regain strength, mobility, and function after surgery. It includes physical therapy, exercises, and treatments tailored to the specific surgery and individual needs.
-
What does a typical post-operation rehab program include?Programs vary but may include: Physical therapy exercises. Manual therapy to improve mobility. Pain management techniques. Education on proper posture and movement. Guidance on gradually resuming daily activities.
-
How can I speed up my recovery during rehab?Follow your therapist’s instructions diligently. Stay consistent with prescribed exercises. Eat a healthy diet to support healing. Avoid overexertion and listen to your body. Stay positive and patient—recovery takes time.
-
How long does post-operation rehabilitation take?The duration depends on the type and complexity of the surgery. Minor procedures may require a few weeks of rehab, while major surgeries, such as joint replacements, may need several months.
-
Will rehabilitation be painful?Some discomfort is normal, especially when working on stiff or weak areas. However, therapy should not cause severe pain. As your therapist, I will adjust the intensity to your comfort level.
-
What surgeries commonly require rehabilitation?Rehab is commonly needed after: Orthopedic surgeries (e.g., knee or hip replacements, rotator cuff repairs). Spinal surgeries. Cardiac surgeries. Abdominal surgeries. Sports-related surgical procedures.
-
Why is post-operation rehabilitation important?Rehabilitation is crucial for: Restoring strength and range of motion. Reducing pain and swelling. Preventing complications like stiffness or scar tissue. Helping patients return to daily activities safely.
5: Dynamic
Assessment
Dynamic movement assessments evaluate an individual's ability to perform movements in motion, such as gait analysis, depth jumps, and the Davies test.
These tests assess coordination, stability, and strength during dynamic activities, identifying imbalances or weaknesses.
They help improve performance, prevent injuries, and guide personalized training and rehabilitation programs.